Attention Deficit Hyperactivity Disorder
Attention Deficit Hyperactivity Disorder
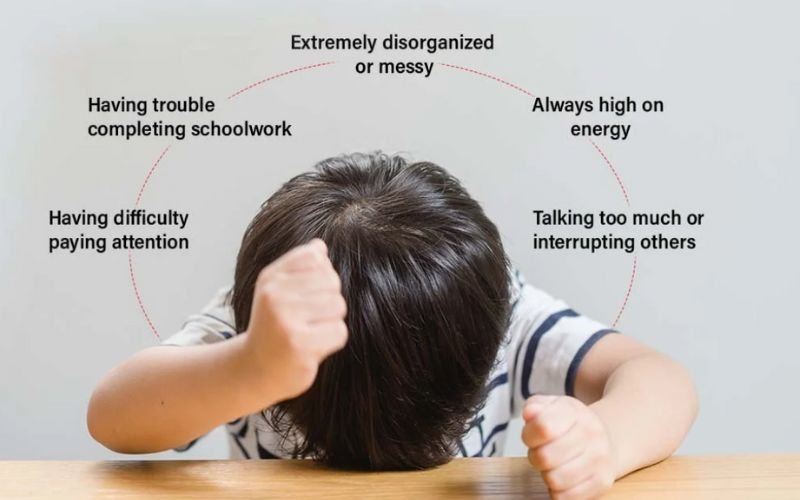
What are the symptoms of ADHD?
What causes ADHD?
- Lead exposure
- Brain anatomy
- Substance use during pregnancy
- Premature birth
- Low birth weight
- Allergies
- Immunizations
- Eating too much sugar
- Excessive screen time
- Poor parenting
- Social factors like poverty
How to get diagnosed with ADHD
If you suspect your child may have ADHD, start by scheduling an appointment with their healthcare provider. A pediatrician or specialist can assess if your child has ADHD using guidelines from the American Academy of Pediatrics, which apply to children ages 4 to 17. Diagnosing ADHD in children under 4 is challenging due to rapid changes in behavior and natural overactivity. Diagnosing ADHD in teenagers can also be difficult due to other conditions like depression or anxiety.
There is no specific test for ADHD. The diagnosis involves several steps and gathering information from multiple sources. Observations from various people in different settings, such as home and school, are crucial.
The people involved in assessing your child’s behavior include:
- You
- Your child
- Your child’s healthcare provider
- Your child’s teachers and school staff
- Other caregivers
Your provider will compare your child’s behavior to that of other children their age. They will use the DSM-5-TR guidelines to diagnose ADHD. According to these guidelines:
- Symptoms must occur in at least two settings (e.g., home, school) and cause dysfunction.
- At least six symptoms must be present.
- Symptoms must significantly impair daily functioning.
- Symptoms must have started before age 12.
- Symptoms must have been present for at least six months.
How is ADHD treated?
Behavioral Therapy:
- For children under 13, parent training in behavior management is recommended.
- For adolescents, other types of therapy like social skills training or executive function training are suggested.
- Behavioral therapy aims to strengthen positive behaviors and reduce unwanted ones. Executive function training focuses on improving organizational skills and self-monitoring.
Medication:
- Medication can help manage ADHD symptoms and improve interactions with others.
- Stimulants: These are the most commonly used and effective ADHD medications, with 70% to 80% of children showing improvement.
- Nonstimulants: These work more slowly and generally have a smaller impact but can last up to 24 hours. They may be added if stimulants are not effective.
- Antidepressants: Not FDA-approved for ADHD but sometimes prescribed alone or with other ADHD medications.